Part 2: Why FeNO first? Spotlight on testing & special cases
In Part 1, we explored the redefined approach to asthma diagnosis under the new NICE/BTS/SIGN guidelines. In Part 2, we dive deeper into the role of Fractional exhaled Nitric Oxide (FeNO) testing, looking at why it is now a frontline diagnostic tool and how it fits into broader asthma care, especially for children and those with occupational risks.
Why is FeNO now highlighted in the new guidelines?
FeNO has always been included in the guidelines and was central to the previous National Institute for Health and Care Excellence (NICE) guidelines for asthma care and management; however, the British Thoracic Society (BTS) and the Scottish Intercollegiate Guidelines Network (SIGN) previously only recommended FeNO to prove an asthma diagnosis. Now, all three have come together and recommended a FeNO test as a first-line diagnostic test for asthma.
Nitric Oxide (NO) is a gas we breathe out all the time; it is a normal part of the respiratory process. When a person has eosinophilic inflammation, more NO is produced, which results in a higher FeNO reading.
Occupational asthma
There is no new update to the guidelines on occupational asthma; the guidelines refer you to the BTS clinical statement for occupational asthma. It does state that if a patient has adult-onset asthma or poorly controlled established asthma, you should check if the symptoms are work-related, by asking the following questions:
- Are your symptoms the same, better or worse on days away from work?
- Are your symptoms the same, better or worse when on holiday or longer than usual breaks from work?
If symptoms worsen at work and occupational asthma is suspected, the patient should be referred to a specialist.
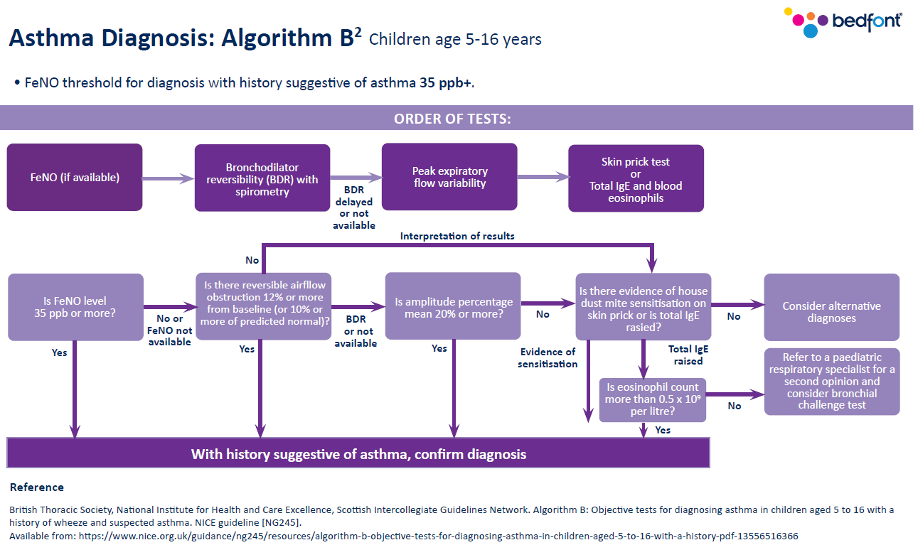
Asthma diagnosis in children (Aged 5-16)
As with adults, once a clear history and physical examination has taken place and asthma is suspected, you can move on to carrying out tests.
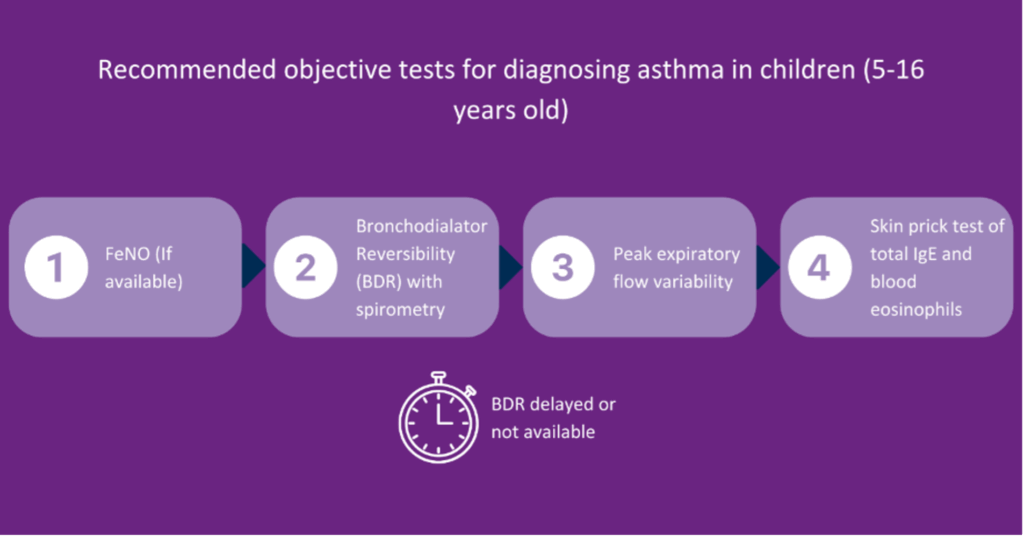
The first and only recommended test for children is a FeNO test. This means that a FeNO device should be available in primary care.
- If the FeNO result does not support an asthma diagnosis, you should move on to bronchodilator reversibility (BDR) with spirometry. However, children on the younger side of the age bracket may find this test very challenging.
- If this is the case, the guidelines recommend you move on to a peak flow diary.
- A skin prick test is recommended if the peak flow diary results do not suggest asthma. Unfortunately, skin prick testing is not widely available, so this may not be possible.
- Blood eosinophils are recommended last due to the invasiveness of the test.
How can you incorporate FeNO testing?
In some Primary Care Networks (PCNs), nursing teams have short slots available daily to perform FeNO tests on the day of presentation. This means the entire nursing team is trained to perform and correctly code a FeNO test and result. This approach, however, is not always possible in some settings, so some will ensure all clinicians are appropriately trained. This means that patients can receive instant results, start treatment immediately in the same appointment, and be referred to the asthma specialist for a follow-up.
Children under 5 years old
Previously, healthcare professionals (HCPs) were told not to diagnose asthma in children under 5 years old; it was recommended that they wait until they were 5 years old to make a diagnosis.
The new guidelines recognise that diagnosing this age group is challenging, as young children do not have the breath control required to take a test.
The recommendations in the new NICE/BTS/SIGN guidelines are:
- If you suspect asthma, use your clinical judgement to treat and review regularly.
- Once the patient reaches 5 years old, attempt to test for asthma. However, it is unclear whether treatment should stop before the test.
- If the test is unsuccessful, continue treatment with regular reviews.
- Re-attempt the tests every 6-12 months.
- If the patient is not responding to treatment, refer them to a specialist, as it may not be asthma.
The guideline also recommends that any preschool child admitted to the hospital or had two or more emergency care visits because of respiratory issues in 12 months be referred to a specialist.
What’s next?
With a clearer understanding of FeNO testing and its applications, we will now focus on how these new guidelines reshape asthma treatment and long-term management. In Part 3, we will cover therapy options across age groups, medication strategies, and key recommendations for improving asthma control.
To keep up to date with our upcoming webinars, please follow us on social media or visit our website here.
