Stoptober takes place every October in the UK. Launched in 2012, the campaign encourages smokers to quit for 28 days. The theme for 2024 is ‘When you stop smoking, good things start to happen’. Bedfont® Scientific Ltd., world leaders in breath analysis, hosted a discussion with Smokerlyzer® Medical Advisory Board Members Dr Amer Siddiq Amer Nordin and Dr Anne Yee. The panel explored the impact Stoptober has on people’s quit smoking attempts as well as, the efforts made in their native Malaysia in regards to smoking cessation.

Dr Amer Siddiq Amer Nordin is an Associate Professor in Psychiatry and Consultant Psychiatrist at the University of Malaya. He is also an Adjunct Professor in Public Health at the Universitas Airlanggar, Surabaya in Indonesia. Additionally, he leads the nicotine addiction research group at the University of Malaya Centre of Addiction Sciences (UMCAS) -NARCC and his research work is primarily on tobacco control and mainly assisting in helping people to quit smoking.
Dr Anne Yee is an Associate Professor at Monash University Malaysia and an Adjunct Professor at UMCAS, University Malaya. Her research is focused on nicotine addiction. She is also currently a Technical and Expert Advisor to the Malaysia Ministry of Health in the development and implementation of the National Clinical Practice Guidelines for Tobacco Use Disorder, mQuit Service Project, Technical Working Group on Evidence-based Smoking Cessation and free tobacco policy at her university.

The discussion covered some interesting subjects around smoking cessation, including Stoptober, smoking cessation efforts in Malaysia, the increasing prevalence of vaping and the role carbon monoxide (CO) devices play in helping individuals quit smoking.
What is Stoptober?
Stoptober is now in its 14th year; this month-long UK public health campaign encourages smokers to quit for 28 days. Research has shown that if you stop smoking for 28 days, you are 5 times more likely to quit for good1. This campaign is designed to make quitting smoking more achievable by providing structured support during October, with the ultimate goal of improving public health.
How have marketing regulations around smoking-related products influenced smoking habits and cessation efforts?
Ultimately, we want people to attempt to quit smoking and the environment around those people to support that attempt. This can be done by:
- Giving people the opportunity to quit,
- Advertise and encourage people to quit,
- Provide people with stop smoking aids

With the resources available, individuals can quit smoking. However, the environment must be pro-quitting. This can be achieved through policies such as no-smoking areas and de-normalising smoking behaviour. This will help people attempting to quit, feel safe to quit and maintain a no-smoking status. This is where Stoptober is a great initiative, promoting smoking cessation and bringing everyone together in their attempt.
The impetus of Stoptober has helped assist people to stop smoking and there are a variety of initiatives within the campaign that are quite useful. Quit smoking aids have been made highly accessible and it has driven healthcare providers to have the materials available to assist people’s quit attempts.
It is estimated that every Stoptober, around 300 – 400 thousand people in the UK attempt to quit smoking2. The campaign creates a sense of community, promoting quitting together with a clear structure of 28 days. These points are what make Stoptober so successful.
Are there any behavioural or psychological mechanisms during Stoptober that increase the chance of stopping smoking for good?
During October, as individuals are driven to quit, they are provided with every opportunity to quit. The digital health programme by the University College London (UCL) empowers those who want to quit on their own to do so, but providing a digital app, means those people are not actually on their own. Those who prefer face-to-face interaction have access to stop-smoking clinics across the country.
Stoptober is supported by the government, which drives an actionable campaign for those who want to quit and quit together in masses. This is where the communal effort is helpful, support from others going through the same experience can help.
A good example of communal effort is Ramadan, Ramadan is an Islamic holy month where Muslims fast from dawn to sunset. As Muslims are required to abstain from smoking during fasting hours, this provides the perfect opportunity for Muslims to quit smoking indefinitely and can act as a natural starting point to quit smoking.
Government-led initiatives should not just be one-offs, there should be regular or continuous efforts. People’s motivation to quit smoking should not just be 1 month of the year, in May we have World No Tobacco Day, which then leads to Stoptober and then leads to the New Year when smokers are inspired to make a change and attempt to quit again if they previously were unsuccessful. Eventually, if the cycle continues, people will be more likely to quit for good.
What is happening in Malaysia concerning smoking cessation efforts?
Coincidentally, Malaysia’s Control of Smoking Products for Public Health Act 2024 officially came into effect in October. This act has stricter regulations on packaging, advertising of smoking and vaping products and public smoking bans.
Malaysia is on track to provide a pro quitting environment and these regulations will help maintain that. This is the first bill of its kind to come into effect and specifically targets the use of e-cigarettes such as vapes among minors; preventing the sale of tobacco and e-cigarettes to minors.
There is a difference between Malaysia and the UK concerning vapes, in the UK, vapes are used to aid smoking cessation. However, in Malaysia, it has been made increasingly more difficult to obtain these devices.

The UK has a goal to be smoke-free by 2030, are there any similar targets in Malaysia?
Malaysia’s goal is to be smoke-free by 2040, reduced from the 2045 date originally set. This allows Malaysia 15 years to plan and strategize how they aim to meet this goal.
Does Malaysia face any unique challenges in comparison to other countries, about reducing smoking rates?
If this question had been asked this time last year, the biggest challenge would have been that Malaysia did not have a Tobacco Control Act, but thankfully this was enforced in October 2024.

There are some unique challenges faced in Malaysia compared to other countries, this is due to the difference in policies. In light of the recent act that has just come into force, the use of electronic cigarettes is now going to be heavily regulated. Although Malaysia has not banned the use of e-cigarettes like some neighbouring countries, the stricter regulations present a challenging position within the region regarding this issue. Hopefully, with the new act in force, things will become a little easier concerning tobacco control.
Whilst there are some unique challenges, Malaysia faces the same barriers as many other countries in reducing smoking prevalence. Smoking rates are higher among individuals from lower socioeconomic backgrounds compared to those from wealthy backgrounds3. There is a link between poverty stress and smoking, making it more difficult for this group to quit, especially as they lack access to smoking cessation clinics, support and resources.
Higher rates of smoking are found among certain populations in Malaysia such as:
- People with mental health conditions,
- The homeless,
- People in prison,
- People who use illicit drugs.
Higher rates of smoking are also found across different regions in Malaysia and this is likely to be down to the difference in funding and resources available in those locations. In rural areas, even if someone wanted to give up smoking, they would find it hard, due to the lack of help in those areas.
The biggest concern currently in Malaysia is the rise of vaping among young people. In 2011, the prevalence of vaping in young people was around 0.8%, rising to 5.8% in 20234. Resources are now being used to encourage this group of people to quit smoking and vaping.
What role do CO monitoring devices play in helping individuals quit smoking and how effective are they as a motivational tool?
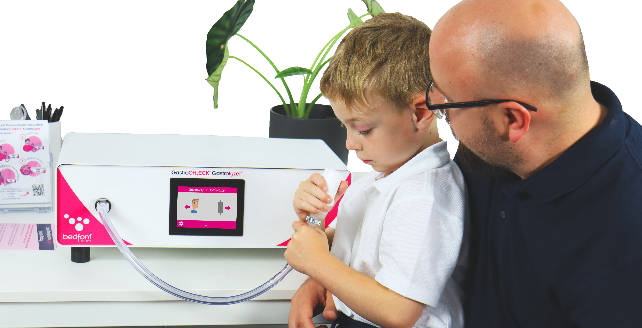
CO devices play an important role in smoking cessation programmes as they offer immediate and tangible feedback to smokers on their CO levels. It is also a key indicator of how smoking impacts the body, providing real-time feedback on the immediate effects of their smoking behaviour. It also shows the results of their daily, weekly and monthly efforts to give up smoking by showing the reduction in CO levels.
Research has shown that those who used a CO device during their quit attempt have higher success rates than those who did not5.
We live in a digital world and these devices have the opportunity to integrate with digital health forms, allowing smokers to monitor their progress over time. The Bedfont® iCOquit® Smokerlyzer® does just that.
Part of the Smokerlyzer® range, the iCOquit® is a personal Bluetooth® CO device that connects to an app and allows users to measure their CO levels remotely whilst quitting smoking. This then allows for the results to be shared with smoking cessation advisors.
People are now moving towards taking control of their health, leading to healthier lifestyles and this is where the iCOquit® can help. Empowering people to take ownership of their health and do something about it, allowing people to quit smoking on their terms, by themselves to a certain extent. To find out more about the iCOquit® and the Smokerlyzer® range, click here.

Malaysia has developed a digital health tool ‘GEMPAQ’ (Getting Every Smoker to Participate and Quit). The app offers smokers a convenient and accessible platform to receive tailored support to help them quit smoking. If this app could be integrated with the Smokerlyzer® devices, it would be a big help to those who want to quit smoking.
In summary, CO devices like the Smokerlyzer® range help to maintain that motivation to keep up with a person’s quit attempt and help them to maintain a no-smoking status. Immediate biofeedback is particularly helpful for some smokers, allowing them to see their quit attempt manifesting positively through the reduction of CO in their respiratory system, which correlates with the improvement of their overall health.
What advice can be given to someone who relapses after Stoptober?
Evidence suggests that the more times you attempt to quit, the more likely it is you will succeed. Stoptober is a great opportunity to re-attempt to quit if a previous attempt has failed earlier in the year.
Both Dr Amer Siddiq Amer Nordin and Dr Anne Yee say “You learn something from each quit attempt, making you stronger to face the next attempt. Each time you gain knowledge and can expand the support network, giving you a better chance of succeeding.”
The discussion covered some very important and interesting topics. To watch the full discussion, see below:
If you enjoyed our expert discussion on Stoptober, be sure to watch our previous discussion on World No Tobacco Day, featuring Dr Amer, Dr Anne and external guest speaker Professor Christopher Bullen.
References
- Gov.uk. Department of Health and Social Care, NHS England and Neil O’Brien MP. [cited on 22/8/24] Available from https://www.gov.uk/government/news/95-of-ex-smokers-see-positive-changes-soon-after-quitting#:~:text=Stoptober%20is%20based%20on%20evidence,likely%20to%20quit%20for%20good.
2. ucl.ac.uk. UCL. [cited on 17/10/24] Available from https://www.ucl.ac.uk/impact/case-studies/2022/apr/ucl-research-informs-stoptober-helping-thousands-quit-smoking
3. BMC Public Health. Hock Kuang lim, Sumarni Mohd Ghazali, Cheong Chee Kee, Kuay Kuang Lim, Ying Ying Chan, Huey Chien The, Ahmad Faudzi Mohd Yusoff, Gurpreet Kaur, Zarinah Mohd Zain, Mohamad Haniki Niki Mohamad & Sallehuddin Salleh. [cited on 16/10/24] Available from https://bmcpublichealth.biomedcentral.com/articles/10.1186/1471-2458-13-8
4. nst.com.my. Hana Naz Harun, Fuad Nizam. [cited on 16/10/24] Available from https://www.nst.com.my/news/nation/2024/05/1051419/600-pct-increase-e-cigarette-users-2023-2011-updated
5. pcrs-uk.org. Noel Baxter. [cited on 16/10/24] Available from https://www.pcrs-uk.org/sites/default/files/CarbonMonoxideTesting.pdf